Facial Fracture & Maxillofacial Trauma Surgery in Sydney and the North Shore
Reconstructive surgery to fix broken facial bones or damaged soft tissues after trauma.
Facial fractures (also called maxillofacial trauma) are among the most serious injuries to the face. They can affect both appearance and essential functions such as chewing, breathing, speech, and vision. They often involve the jaw, cheekbone, nose, or eye socket. Timely assessment and treatment are critical to improve function and appearance.
As a FRACS-qualified Specialist Plastic Surgeon, Dr Varun Harish is frequently consulted as a facial trauma surgeon in Sydney and maxillofacial trauma surgeon on the North Shore, treating complex jaw, cheekbone, eye socket and nasal fractures. He consults in St Leonards and operates at Royal North Shore, Mater and North Shore Private Hospitals, where urgent cases such as broken jaws, cheekbone fractures, orbital (eye socket) injuries, and nasal fractures are treated. Patients are commonly referred by GPs, emergency departments and specialists from across Sydney and the North Shore.
If you or your patient has sustained a facial injury — such as a broken jaw, fractured cheekbone, or eye socket trauma — urgent assessment is recommended. Our team can arrange consultation and appropriate treatment.

Understanding Facial Fractures
Urgent Appointments for Facial Fracture Surgery in Sydney’s North Shore
Facial fractures and maxillofacial injuries require urgent attention to prevent long-term problems. If you have suffered a broken jaw, cheekbone, nose or eye socket, contact us. Urgent trauma cases are prioritised, and our team will guide you on what to do next.
Dr Harish treats urgent trauma cases at Royal North Shore, Mater and North Shore Private Hospitals, ensuring access to specialist care across Sydney’s North Shore.
Because this surgery is considered medically necessary, Medicare rebates and private health insurance usually apply.

Common Causes of Facial Fractures & Maxillofacial Trauma
Facial fractures may occur after high-impact trauma, but can also result from everyday incidents. They affect patients of all ages and may happen unexpectedly in both recreational and occupational settings.
Typical causes include:
- Sports injuries – football, rugby, boxing, martial arts
- Motor vehicle accidents – car, motorbike and cycling crashes
- Falls – in children, older adults, or in workplaces
- Assaults – direct trauma to the jaw or midface
- Workplace accidents – industrial or construction-related injuries

If you’ve experienced one of these events and suspect a fracture, urgent assessment is recommended.
Sports-Related Facial Fractures and Injuries
Contact sports are a common cause of facial fractures. Injuries can occur in football, rugby, boxing, martial arts and other activities where the face is exposed to impact.
Common sports-related injuries include:
- Broken jaw (mandible fractures): often from a direct blow during rugby, football or combat sports.
- Broken cheekbone (zygoma): can happen after tackles, punches or collisions.
- Broken eye socket (orbital) injuries: more frequent in boxing and martial arts where the eye is vulnerable.
Prompt treatment of sports-related facial fractures helps reconstruct the injury, reduce the risk of long-term problems, and allow a safer return to activity.

If you have sustained a sports injury in Sydney or on the North Shore and suspect a broken jaw, cheekbone, nose or eye socket, seek urgent assessment. Early management improves outcomes and may help prevent complications.
Symptoms That Need Urgent Review
Certain symptoms suggest a facial fracture or maxillofacial trauma requires urgent treatment. These include:
- Jaw not lining up or bite feels uneven
- Double vision or a sunken eye
- Crooked or flattened nose after injury
- Inability to open or close the mouth normally
- Persistent nosebleeds, swelling or facial numbness
- Changes in breathing after nasal injury
- Bleeding
Prompt treatment can prevent complications and ensure the best chance of full recovery.





If you experience these symptoms, early treatment may improve outcomes. Contact our office to schedule your appointment.
Surgical Details
Why Surgery May Be Needed
Surgery may be required for facial fractures and maxillofacial trauma in order to:
- Reduce long-term risks such as pain or deformity
- Restore facial appearance and symmetry
- Protect vital functions such as chewing, breathing and vision
- Ensure bones heal in the correct position (to prevent them healing incorrectly)
- Correct the bite (occlusion) and jaw function
- Protect the eye/orbit and the airway/nasal passages
Common Facial Injuries & Fractures Treated in Sydney (Broken Jaw, Cheekbone, Eye Socket, Nose)
Facial fractures, also called maxillofacial trauma, can affect different bones of the face, and each fracture requires a tailored surgical approach. The most common fractures are outlined below, with information about symptoms, surgical treatment, and where incisions are usually placed. Dr Harish provides urgent treatment for patients with broken jaws, broken cheekbones, broken noses, and injuries to the bones around the eye.
Eye Socket Injury (Orbital Fracture Repair in Sydney and the North Shore)
Orbital fractures affect the bones that form the eye socket. Because the orbit protects the eye, these injuries can impact both vision and the position of the eye. Prompt treatment helps prevent long-term issues with eyesight and appearance.
Common symptoms include:
- Double vision
- Sunken appearance of the eye
- Difficulty moving the eye
- Numbness around the cheek or forehead
- Swelling and bruising around the eye
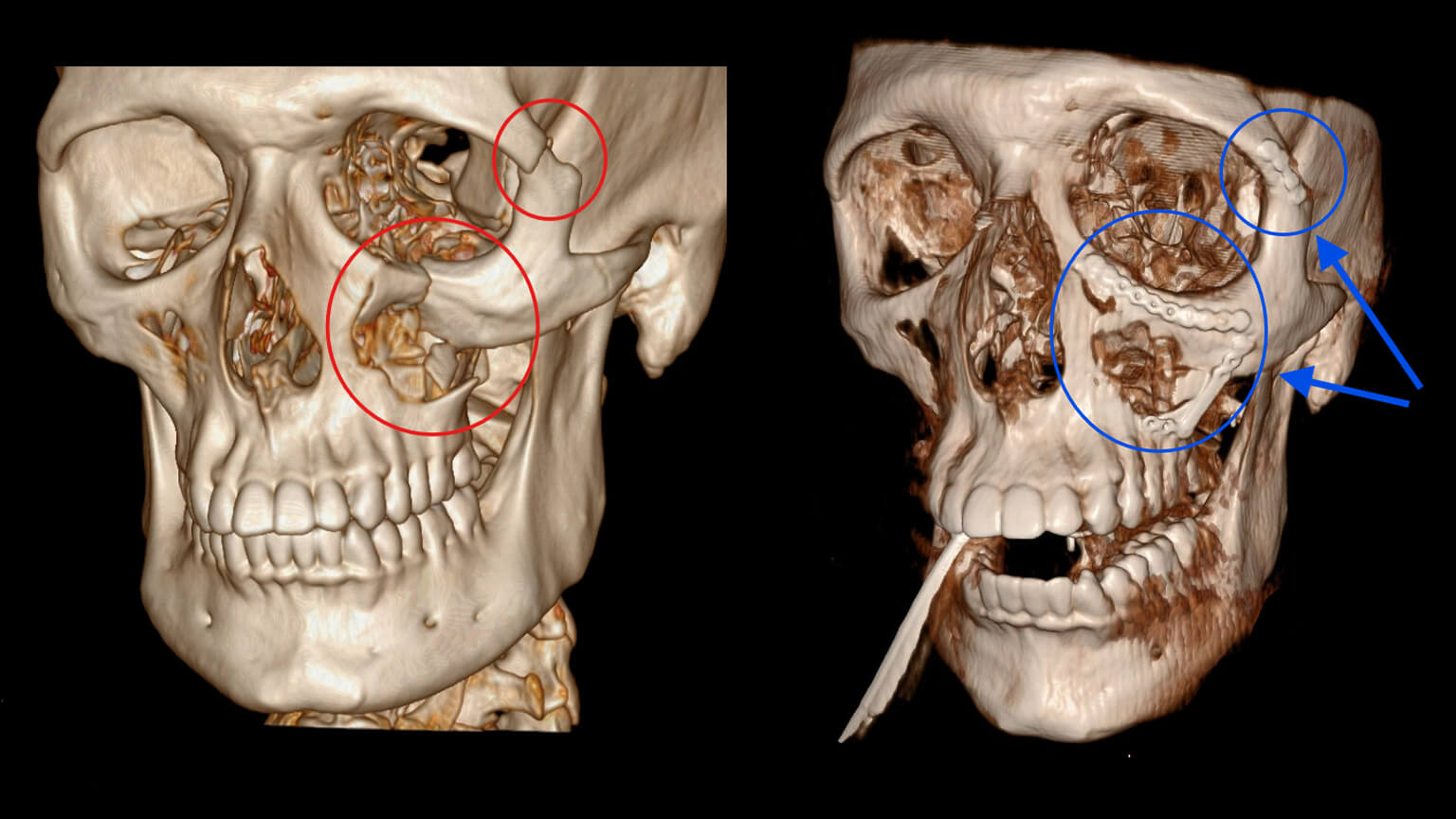
Surgical treatment usually involves stabilising the broken eye socket walls with titanium mesh, and repositioning eye socket contents. This helps restore normal eye position and function.
Incisions are typically hidden within eyelid creases or the conjunctiva (inner aspect of the eyelid), leaving little to no visible scarring.



Broken Cheekbone (Zygomatic Fracture Surgery in Sydney and the North Shore)
The zygoma, or cheekbone, is central to the shape and symmetry of the face. When fractured, it can affect not only appearance but also the function of the eye socket. Surgical treatment restores balance and prevents lasting deformity.
Common symptoms include:
- Flattening of the cheek
- Swelling and bruising around the cheek and eye
- Difficulty opening the mouth
- Numbness below the eye or upper lip
Surgical treatment involves repositioning the cheekbone and fixing it with small titanium plates and screws to restore facial symmetry.
Incisions are usually placed inside the mouth, at the temple, or within the lower eyelid crease, making scars as discreet as possible.

Broken Jaw (Mandible Fracture Surgery in Sydney and the North Shore)
The mandible, or lower jaw, plays a vital role in chewing, speaking, and facial profile. A fractured jaw can cause pain, difficulty eating, and an uneven bite. Surgery aims to restore both function and appearance.

Common symptoms include:
- Jaw pain and swelling
- Difficulty chewing or opening the mouth
- Teeth not lining up properly (malocclusion)
- Numbness of the lower lip or chin
Surgical treatment usually involves open reduction and internal fixation with titanium plates and screws. In some cases, the jaw may need to be immobilised temporarily. Patients often follow a soft or liquid diet during healing.
Incisions are most often placed inside the mouth to avoid visible scars, though occasionally an external incision may be required.


Broken Nose (Nasal Fracture Surgery & Correction in Sydney)
Nasal fractures are the most common type of facial fracture. Because the nose is central to both appearance and breathing, timely treatment is important to ensure normal airflow and prevent long-term cosmetic concerns.
Common symptoms include:
- Pain and tenderness over the nose
- Swelling and bruising around the nose and eyes
- Crooked or flattened nasal bridge
- Nosebleeds
- Difficulty breathing through the nose
Treatment may involve closed reduction, which repositions the nasal bones without open surgery, or open repair in more complex cases.
Comprehensive Maxillofacial Trauma
In some cases, patients may suffer severe facial injuries that involve more than one bone of the face. These complex injuries are sometimes called midface fractures or Le Fort fractures, and they may affect the upper jaw, cheekbones, and eye sockets at the same time.
Other patients suffer injuries to the upper face, including the frontal bone (forehead) and the bones just above the eye sockets. These fractures are often caused by high-energy accidents and can involve the frontal sinus. Treatment requires specialist surgery to protect the brain, restore the forehead shape, and maintain the function of the sinuses and eye sockets.
Dr Harish provides comprehensive management of upper face, midface and panfacial fractures as part of his expertise in maxillofacial trauma surgery in Sydney and across the North Shore.

Surgical Procedures
Surgical treatment for facial fractures and maxillofacial trauma begins with a thorough consultation and CT imaging to understand the extent of the injury.
Surgery is performed under general anaesthesia. The fractured bones are repositioned and stabilised using small titanium plates and screws. These plates are safe, biocompatible, and usually remain permanently in place without causing issues.
Wherever possible, incisions are hidden inside the mouth or within natural skin creases such as the eyelid. This helps to minimise visible scarring. Dissolvable stitches are used in most cases, and antibiotics are prescribed to reduce the risk of infection.
In complex facial fractures, advanced imaging can now be used during surgery to make treatment even more precise. Dr Harish has published research in the Australasian Journal of Plastic Surgery (2024) showing how intraoperative CT scans (iCT) give the surgeon a clear “real-time picture” while operating. This means your fractures can be checked and adjusted on the spot, reducing the chance of needing a second operation and helping you recover with more confidence in the result. Read the study here.

Practical Information
Recovery & Results
Week 1
Swelling and bruising peak. Pain is managed with medication and cold compresses.
Weeks 2–3
Stitches are removed if present, and swelling begins to settle. Patients often resume light daily activities at this stage.
Weeks 6–12
The bones continue to heal. Most patients return to work or school, with function steadily improving.
3–6 months
Final healing occurs, with restoration of facial appearance and function.

Recovery is generally better when treatment is provided promptly, though outcomes vary.
Risks & Safety
Facial fracture and maxillofacial trauma surgery in the hands of a Specialist Plastic Surgeon experienced in maxillofacial trauma is considered safe. Serious complications are uncommon. Possible risks include:
- Bleeding or infection (rare, and usually managed effectively)
- Temporary numbness or altered sensation in the lips, cheek or chin
- Bones healing in the wrong position if treatment is delayed or if healing is abnormal
- Very rare need for revision surgery
Costs & Insurance
Facial fracture surgery is generally considered medically necessary. This means Medicare and health funds typically contribute to the costs of treatment. The exact amount depends on your level of cover, the hospital fees, the type of fracture, and the complexity of the surgery.
Dr Harish and his team will provide a detailed cost estimate at your consultation and guide you through Medicare and insurance entitlements.
Frequently Asked Questions
How soon should facial fractures be treated?
Most fractures are ideally treated within two weeks before bones begin to heal incorrectly.
Do all facial fractures need surgery?
Not all fractures require surgery. Small or stable fractures may heal without surgery, but displaced or complex fractures usually require surgical repair.
What is facial trauma or maxillofacial trauma surgery?
Maxillofacial trauma surgery refers to the treatment of serious injuries to the face, including broken jaws, cheekbones, eye sockets, and nasal bones. It restores both function and appearance after trauma. Dr Varun Harish is a facial trauma surgeon in Sydney and maxillofacial trauma surgeon on the North Shore, with expertise in repairing broken jaws, cheekbones, eye sockets and noses.
Will I have visible scars?
Most patients have little to no visible scarring, as incisions are hidden in natural creases. Incisions are usually hidden inside the mouth, eyelid creases, or remotely away from fractures, leaving minimal visible scarring.
How long is recovery?
Most patients recover within 6–12 weeks, though final healing can take up to 6 months. Most patients resume light activities within 2–3 weeks, while complete bone healing can take upwards of 6 weeks.
Is the surgery covered by insurance?
Yes, facial fracture surgery usually attracts rebates by Medicare and health funds.
When can I return to work or school?
Most patients return to desk-based work or school within 2–3 weeks, while physical jobs may require 6–8 weeks.
When can I play sport again?
Light exercise may resume after 3–4 weeks. Contact sports should be avoided for at least 6 weeks to protect healing bones.
Can old fractures be corrected?
Yes, old fractures can often be corrected. Revision surgery can improve both function and appearance, even months or years after the initial injury.
What happens if a facial fracture is left untreated?
Untreated fractures can result in long-term deformity, chronic pain, vision problems, breathing difficulties, and impaired jaw function.
Will I need plates or screws in my face?
Titanium plates and screws are commonly used to hold fractured bones still as they heal. They are safe, biocompatible, and usually remain in place permanently.
Can plates or screws be felt under the skin?
In most cases, plates and screws are not noticeable. Rarely, if they cause discomfort, they can be removed once healing is complete.
When can I drive again after facial fracture surgery?
Most patients can safely drive again after 1–2 weeks. You can usually drive once you are no longer taking strong pain medication and can comfortably turn your head and react quickly.
Will my face look normal again after surgery?
Many patients experience restoration of appearance and function, though outcomes depend on the injury.
Are facial fractures common in children?
Yes, children can sustain facial fractures, although their bones heal faster than adults. Special care is taken to avoid affecting future growth.
What symptoms suggest facial fractures or maxillofacial trauma need urgent review?
Seek urgent review if you notice a crooked or flattened nose, double vision, a sunken eye, your jaw not lining up, numbness in the face or lips, or difficulty opening or closing the mouth normally.
How much does facial fracture or maxillofacial trauma surgery cost?
Facial fracture surgery is generally considered medically necessary. This means Medicare and health funds typically contribute to the costs of treatment. The exact amount depends on your level of cover, the hospital fees, the type of fracture, and the complexity of the surgery. You will receive a detailed cost estimate at your consultation.
Is facial fracture surgery painful?
Most patients experience some discomfort, swelling, and bruising in the first week, but pain is usually well controlled with prescribed medications. Discomfort improves steadily as healing progresses.
Will I need revision surgery?
Most fractures heal well with initial surgery, but a small number of patients may require a second procedure if bones heal incorrectly or hardware causes problems.
Can children have surgery for facial fractures or maxillofacial trauma?
Yes. Children’s bones heal quickly, and surgery is performed with special care to protect facial growth and development.
About Dr Harish
Why Choose Dr Varun Harish
- Fellow of the Royal Australasian College of Surgeons (FRACS)-qualified Specialist Plastic Surgeon
- Australian Society of Plastic Surgeons (ASPS) member
- Extensive experience in facial fracture and maxillofacial trauma surgery
- Operates at Royal North Shore, Mater, and North Shore Private Hospitals
- Internationally published on complex facial fracture management and intraoperative CT imaging (Australasian Journal of Plastic Surgery, 2024), contributing to best-practice standards in maxillofacial trauma care.
- Treats both emergency trauma and revision of old fractures
- Trusted by patients across Sydney’s North Shore including Chatswood, Mosman, North Sydney, and the Northern Beaches
For patients concerned about scars after fracture repair, Dr Harish also offers Scar Revision Surgery.
Book a Facial Fracture Consultation
If you have suffered a facial injury, don’t delay. Early treatment of facial fractures and maxillofacial trauma gives the best chance of recovery.

Serving Sydney and the North Shore
Dr Varun Harish provides urgent facial fracture and maxillofacial trauma surgery in Sydney’s North Shore, with patients attending from across the region.
Patients visit our St Leonards clinic from:
Lower North Shore
Crows Nest, North Sydney, Neutral Bay, Mosman
Central North Shore
Chatswood, Lane Cove, Ryde, Killara
Upper North Shore
Hornsby, Wahroonga, Turramurra, St Ives
Northern Beaches
Manly, Dee Why, Mona Vale
Inner West
Ashfield, Burwood, Newtown
North West
Castle Hill, Baulkham Hills
Central Coast
Gosford, Terrigal, Woy Woy
Our clinic is located beside Royal North Shore Hospital and within easy reach of St Leonards Station and Crows Nest Metro. Secure parking options are available nearby, making it convenient for patients across Sydney to attend consultations and follow-up appointments.
By choosing Dr Harish — an experienced FRACS-qualified reconstructive surgeon — for facial fracture surgery in Sydney, you can access precise, evidence-based treatment with a focus on restoring both function and appearance.
