
Facial Fractures Explained — How They’re Treated and When Surgery Is Needed
Dr Varun Harish, FRACS Plastic Surgeon
First published:
Understanding Facial Fractures
A facial fracture means that one or more of the bones forming the face have broken. Facial bones form the structure of your features, protect vital areas like the eyes, nose and mouth, and help with chewing, breathing and facial expression. When a fracture occurs, it can cause swelling, bruising, pain or changes in facial shape — but most injuries can be repaired safely once swelling settles.
Most facial fractures are not life-threatening, but some can affect vision, breathing, or bite alignment if not assessed and managed appropriately. You may find out you have a broken face after an emergency department visit or a CT scan, or when swelling, bite changes, or double vision persist after trauma to the face.
Other signs that may be important include ongoing numbness in the cheek, upper lip or teeth, difficulty opening the mouth, or a change in facial shape as swelling settles. If there is heavy bleeding, trouble breathing, or a sudden change in vision, urgent medical care is needed.

What to Do After a Facial Injury
- Seek prompt medical review, even if symptoms seem mild. Early assessment helps identify fractures and prevents complications.
- Apply a cold compress to reduce swelling.
- Avoid blowing your nose if the nose or eye socket may be injured — this can push air into soft tissues and worsen swelling.
How Facial Fractures Happen
Facial fractures usually result from:
- Falls — especially in older adults or during contact sports
- Motor-vehicle accidents — a common cause of multiple fractures
- Workplace incidents or sporting collisions
- Assaults or other blunt impacts
In New South Wales, many injuries from work or road accidents are managed under WorkCover or Compulsory Third-Party (CTP) insurance schemes; referrals usually come through hospital emergency departments or a GP.
Types of Facial Fractures
| Fracture site | Typical symptoms |
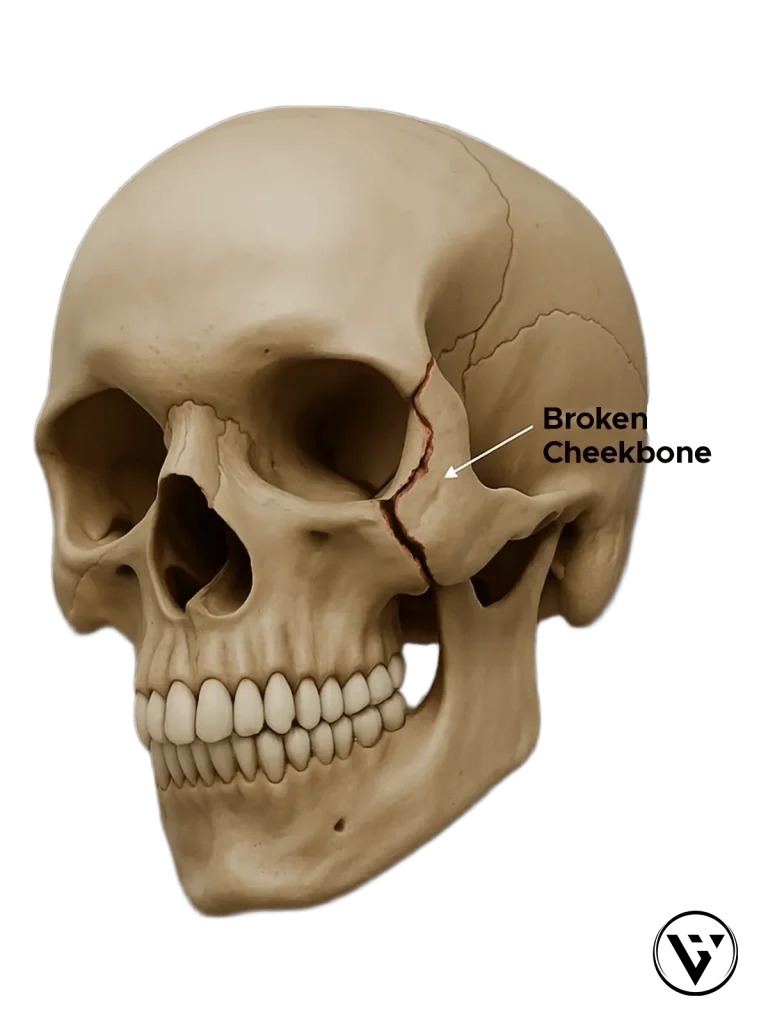
| Zygomatic fracture (broken cheekbone) | Flattened cheek, bruising around the eye, difficulty opening the mouth |
| Orbital fracture (broken eye socket) | Double vision, pain with eye movement, eye appearing sunken or out of position |
| Mandibular fracture (broken jaw) | Bite feels off (teeth don’t meet normally), pain when chewing, restricted movement |
| Nasal fracture (broken nose) | Nosebleed, crooked appearance, breathing change |
| Complex / multiple fractures | Combination injuries from high-energy trauma with swelling or asymmetry (two sides don’t match) |
How a Diagnosis Is Made
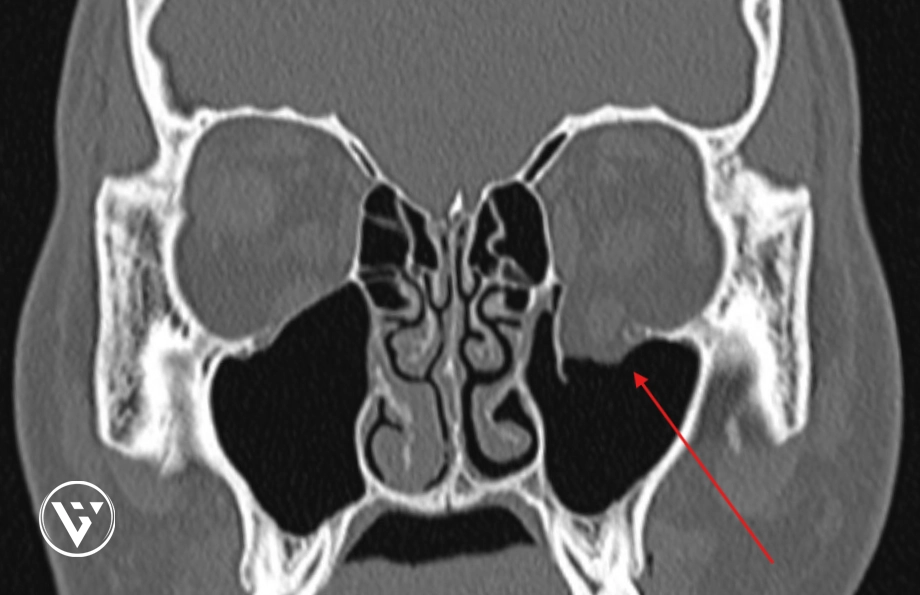
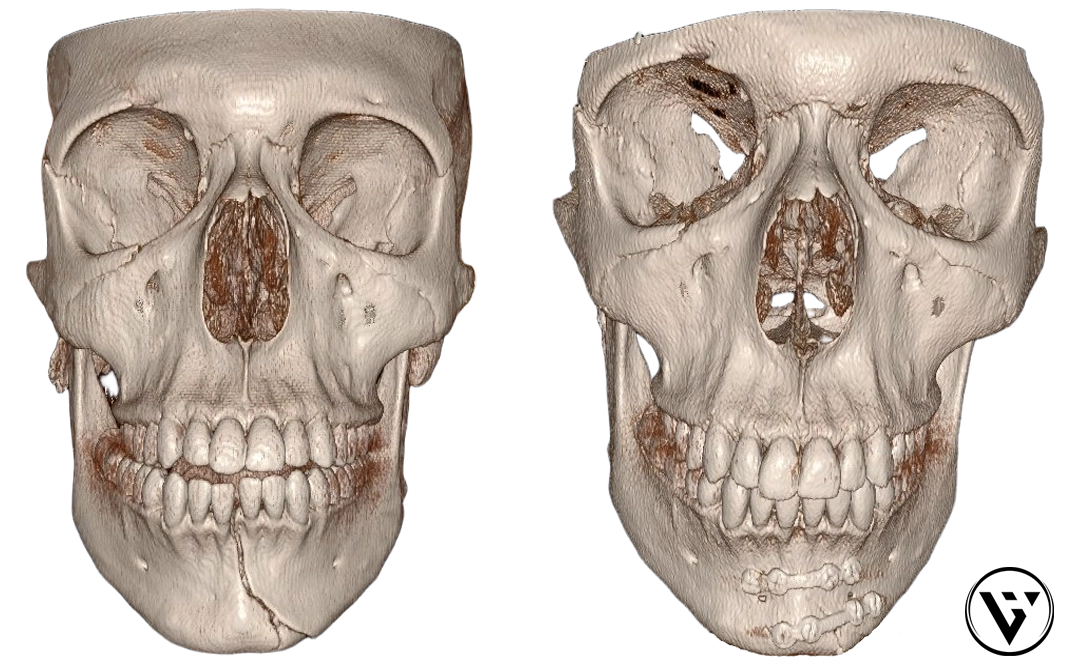
A CT scan is a special type of X-ray that creates 3D pictures of the facial bones. This shows exactly where the break is and whether any pieces have moved.
A CT scan also shows how bones may have shifted. For example, it might show whether the thin bone beneath the eye (orbital floor) has been affected (often called a ‘blow-out’ or ‘blow out’ fracture). All of this information helps guide whether observation or surgery is likely to be beneficial.
At major trauma centres where Dr Varun Harish works including Royal North Shore and Liverpool Hospitals, these scans are reviewed by team-based trauma services, typically involving Plastic and Reconstructive Surgeons in facial bone and soft-tissue repair, to plan the safest repair.
When Surgery Is Needed — and When It’s Not
Some fractures do not need an operation.
- Non-displaced fracture: the bone has cracked but stayed in a good position – this often heals with supportive non-surgical care.
- Displaced fracture: bone pieces have moved out of position – may need surgery to reposition and hold them still while they heal.
The decision to recommend surgery, however, is based on the individual’s function, bone alignment, and long-term facial stability rather than the fracture alone. Not all fractures benefit from surgery, and unnecessary intervention can introduce avoidable risks.
Surgery is often timed once swelling has settled but before bones begin to heal in the wrong position, which can make later correction more complex. If surgery is recommended, two main approaches are used:
- Closed reduction: gently move the bone back into place without any cuts.
- Open reduction and internal fixation (ORIF): make a small cut, line the bone up again, and secure it with tiny plates and screws (fixation).
The goal of surgery is to restore normal alignment and function while minimising long-term consequences like bite disturbances. Because facial fractures involve both bone and overlying soft tissues, management often considers facial balance, scar placement, and long-term appearance alongside bone healing.
Sometimes an intra-operative CT scan (performed during surgery) is used to confirm the bones are aligned correctly before the operation finishes. Dr Varun Harish’s research published in the Australasian Journal of Plastic Surgery described how this technology can help surgeons check the accuracy of bone positioning and fixation in complex facial fractures.
Operations are usually performed within the first week, once swelling has reduced enough to allow safe and precise repair.
Assessment and treatment can differ in children, as growing facial bones may heal differently from those in adults.
For detailed information on facial fracture or maxillofacial trauma surgery (including cheekbone and orbital surgery) and recovery timelines, visit our Facial Fracture Repair page.
Even if diagnosis is delayed, later reconstruction can still restore comfort and symmetry.
Who Treats Facial Fractures?
Facial fractures are managed by several specialist teams — most often Plastic and Reconstructive Surgeons, Oral and Maxillofacial Surgeons, and Ear, Nose & Throat (ENT) or Ophthalmic Surgeons, depending on which bones and structures are affected. Each brings different expertise to the shared goal of helping restore comfort, balance, and facial function.
Plastic and Reconstructive Surgeons are trained to care for the whole face — repairing broken bones as well as treating the skin, muscles and soft tissues that cover them. Their work aims to recreate the natural form and function of the face, which may include repairing cuts, repositioning and fixing bones, and reconnecting nerves when required. Plastic surgeons also prioritise the cosmetic aspects of facial trauma, aiming for discreet, low-visibility scars and using minimally invasive techniques whenever it is safe and appropriate.
In many trauma centres, Plastic & Reconstructive Surgeons work side-by-side with Maxillofacial, ENT and Ophthalmic specialists, sharing planning and procedures to achieve coordinated care for each patient.
Learn more about Dr Harish’s reconstructive and trauma experience here.
Recovery and What to Expect
- Hospital stay: one to two nights is typical.
- Swelling: peaks at 48 hours and fades over two to three weeks. Sleeping with your head elevated on two pillows can help reduce swelling faster.
- Plates and screws: made of medical-grade titanium, stay permanently, are not felt, and don’t set off airport scanners.
- Numbness: can occur if a nerve is bruised but usually improves over months.
- Scars: positioned inside the mouth or along natural skin folds to be less noticeable.
Avoid smoking while healing, as it can delay recovery.
Follow-up visits are typically at two and six weeks, then around three months.
If any swelling or scarring remains noticeable, scar revision surgery may be discussed.
You can also read about surgical treatment and long-term recovery on our Facial Fracture Repair page.
Returning to Normal Activities
Most people can return to desk-based work within one to two weeks after surgery. Contact sport or heavy lifting is usually delayed for six to eight weeks while the bones regain strength.
Your surgeon will confirm when it’s safe to resume driving, gym workouts or sport.

If you’ve sustained a facial injury or have concerns about your recovery, contact our St Leonards practice for assessment and guidance.
Key Takeaways
- “Fracture” = broken bone.
- CT scans help determine if surgery is required.
- Surgery realigns and stabilises bones using tiny plates and screws.
- Some fractures heal without surgery.
Frequently Asked Questions
What is a facial fracture?
A facial fracture is a broken bone in the face — most often the cheekbone, eye socket, jaw or nose.
Will I need metal plates?
Many repairs use small titanium plates and screws to hold the bones while they heal. They stay permanently and are rarely noticed.
Can a facial fracture heal without surgery?
Yes. If the bone has cracked but remains in a good position (non-displaced), it can heal naturally.
Will my face look normal again?
Most people regain their usual appearance once swelling subsides.
How long does recovery take?
Swelling improves within weeks, but full healing can take several months.
Will I have visible scars?
This depends on the broken bone. Incisions might be placed inside the mouth for jaw fractures, along natural folds to minimise visibility for eye socket fractures or in the hairline for cheekbone fractures.
Is it safe to fly after a facial fracture?
This is dependent on the type and location of the broken bone(s). In some cases, flying may be safe once you have been assessed and serious complications have been excluded. In others, air travel may be delayed if there are broken bones around your sinuses, significant swelling, or trapped air beneath the skin, as pressure changes can worsen discomfort or swelling.
Your treating team can advise on appropriate timing based on the type of fracture, CT findings, and whether surgery is planned.
Can facial fractures be missed at first?
Yes. Swelling can make it hard to assess the face immediately after an injury, and some fractures are not obvious on examination alone. If symptoms persist or there are concerns about alignment, bite, or vision, a CT scan is often used to clarify the injury.
About Dr Varun Harish FRACS
Specialist Consultant Plastic, Reconstructive & Burns Surgeon working in major trauma centres in Sydney – Royal North Shore & Liverpool Hospitals.
Consulting in St Leonards on Sydney’s North Shore, serving patients across the Northern Beaches, Inner West and Central Coast.
Published author on using advanced scanning technologies to improve the accuracy of treatment of facial fractures.

If you’ve been referred after a facial injury or need specialist follow-up after hospital treatment, consultations are available in St Leonards for patients from across Sydney’s North Shore, Northern Beaches, Inner West and Central Coast.
Educational information prepared by Dr Varun Harish FRACS, Specialist Plastic, Reconstructive & Burns Surgeon – Sydney.
Serving patients across the North Shore, Northern Beaches, Inner West and Central Coast.
Last reviewed February 2026.
Read how this site’s medical content is prepared and reviewed
